Waning Immunity Against Japanese Encephalitis Worsens Dengue
Background
-
Dengue and Japanese Encephalitis Virus (JEV) are both flaviviruses (genus Orthoflavivirus).
-
Prior exposure to one flavivirus can influence outcomes of infection with another due to antibody-dependent enhancement (ADE)
-
People in Asia often get vaccinated for JEV.
-
Dengue, however, is spreading fast due to climate change, urbanisation, and travel.
Major diseases caused by members of the family Flaviviridae:
-
Dengue fever
-
Hepatitis C
-
Japanese encephalitis
-
Kyasanur Forest disease
-
Murray Valley encephalitis
-
St. Louis encephalitis
-
Tick-borne encephalitis
-
West Nile encephalitis
-
Yellow fever
-
Zika fever
The study
-
Dharan, Nepal (2019–2023 dengue outbreaks).
-
Why Nepal?
-
Strong JE vaccination since 2006 (so high JEV immunity).
-
Until recently, little exposure to dengue → perfect setting to study the role of JEV immunity.
-
-
Participants: 546 dengue patients (ages 15–65).
-
Researchers measured:
-
Antibody levels against JEV.
-
Severity of dengue infection (using a marker called chymase, which rises in severe dengue).
-
Key Findings
-
61% of patients already had antibodies from JE vaccination.
-
People with medium-level JEV antibodies (not too high, not too low) were more likely to develop severe dengue.
-
They had higher chymase levels (marker of severity).
-
Their risk of “dengue with warning signs” was 3 times higher.
-
-
This effect was independent of prior dengue infection, proving it was linked to JEV immunity alone.
-
This pattern is similar to what scientists saw earlier with Zika and dengue:
-
Very high antibodies = protective.
-
Medium antibodies = dangerous (can actually help dengue virus infect cells → called antibody-dependent enhancement).
-
Why this happens
-
JE antibodies slowly wane over years after vaccination.
-
After ~5 years, only ~63% of people still have protective antibody levels.
-
When antibodies drop to that “middle zone,” instead of protecting, they may worsen dengue infection.
Implications
-
JE vaccination is still very important – it reduced Japanese Encephalitis cases hugely.
-
But we may need timely booster doses of the JE vaccine:
-
To maintain long-term protection against JE.
-
To also reduce the risk of severe dengue in dengue-prone regions.
-
-
Chymase biomarker could help doctors identify patients who are at higher risk of severe dengue early.
-
Shows how different viruses interact inside the human body → one vaccine’s immunity can affect another disease.
-
For countries like India, with both JE vaccination and rising dengue outbreaks, this is a warning to prepare strategies (like boosters + surveillance).
Japanese Encephalitis Virus (JEV):
-
Type: Mosquito-borne flavivirus (related to dengue, Zika, yellow fever, West Nile).
-
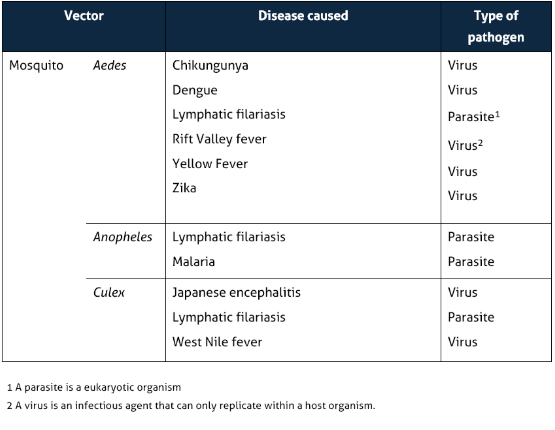
Vector: Culex mosquitoes, especially Culex tritaeniorhynchus.
-
Reservoir hosts: Pigs and water birds (enzootic cycle).
-
Geography: 24 countries in SE Asia & Western Pacific; >3 billion people at risk.
-
First case documented: 1871 in Japan.
Burden
-
Age group: Majority in children <15 years.
-
Fatality rate: Up to 30% of symptomatic cases.
-
Sequelae: 30–50% survivors develop permanent neurological, cognitive, or behavioural disabilities.
Q. How is Japanese encephalitis transmitted?
A. By rice field breeding mosquitoes (primarily the Culex tritaeniorhynchus group) that become infected with Japanese encephalitis virus (a flavivirus antigenically related to St. Louis encephalitis virus).
Q. How do people get Japanese encephalitis?
A. By the bite of mosquitoes infected with the Japanese encephalitis virus.
Q. What is the basic transmission cycle?
A. Mosquitoes become infected by feeding on domestic pigs and wild birds infected with the Japanese encephalitis virus. Infected mosquitoes then transmit the Japanese encephalitis virus to humans and animals during the feeding process. The Japanese encephalitis virus is amplified in the blood systems of domestic pigs and wild birds.
Q. Could you get the Japanese encephalitis from another person?
A. No, Japanese encephalitis virus is NOT transmitted from person-to-person. For example, you cannot get the virus from touching or kissing a person who has the disease, or from a health care worker who has treated someone with the disease.
Q. Could you get Japanese encephalitis from animals other than domestic pigs, or from insects other than mosquitoes?
A.No. Only domestic pigs and wild birds are carriers of the Japanese encephalitis virus.
Q. What are the symptoms of Japanese encephalitis?
A. Mild infections occur without apparent symptoms other than fever with headache. More severe infection is marked by quick onset, headache, high fever, neck stiffness, stupor, disorientation, coma, tremors, occasional convulsions (especially in infants) and spastic (but rarely flaccid) paralysis.
Q. What is the incubation period for Japanese encephalitis?
A. Usually 5 to 15 days.
Q. What is the mortality rate of Japanese encephalitis?
A. Case-fatality rates range from 0.3% to 60%.
Q. How many cases of Japanese encephalitis occur in the world and the U.S.?
A. Japanese encephalitis is the leading cause of viral encephalitis in Asia with 30-50,000 cases reported annually. Fewer than 1 case/year is reported in U.S. civilians and military personnel traveling to and living in Asia. Rare outbreaks in U.S. territories in Western Pacific have occurred.
Q. How is Japanese encephalitis treated?
A. There is no specific therapy. Intensive supportive therapy is indicated.
Q. Is the disease seasonal in its occurrence?
A. Seasonality of the illness varies by country
Q. Who is at risk for getting Japanese encephalitis?
A. Residents of rural areas in endemic locations, active duty military deployed to endemic areas, and expatriates who visit rural areas. Japanese encephalitis does not usually occur in urban areas.
Q. Is there any vaccine available against JE virus in India?
A. Inactivated Mouse Brain-Derived JE Vaccine is available against JE in India. The Vaccine is prepared by subjecting the mouse brain infected with Nakayama strain of JE virus to a sequence of protamine sulphate treatment, formalin inactivation and ultrafilteration and ammonium sulfate precipitation. The purified product is without myclin basic protean and supplied in a freeze dried form. The Vaccine in manufactured at Central Research Institute, Kasauli, Himachal Pradesh
Q. Who should be vaccinated against Japanese Encephalitis?
A. Seroprevalance studies disclose nearly universal infection by early adulthood and in areas where viral transmission is particularly intense Seroprevalance rates may increase during childhood. The age group for immunization should be decided based on available Sero-epidemiological data from the area.
