Antibiotic Culture in India and Its Implications for Mental Health
1. Introduction
-
India is one of the world’s largest consumers of antibiotics.
-
While Antimicrobial Resistance (AMR) is recognised as a major public health threat, its impact on mental health via the gut-brain axis remains underexplored.
-
The problem is compounded by easy access, self-medication, and unregulated prescriptions in India.
2. The Gut-Brain Axis and Mental Health
-
The gut microbiota regulates neurotransmitters like serotonin and dopamine, influencing mood, stress response, and cognition.
-
Antibiotics disrupt this microbiota balance (dysbiosis), leading to:
-
Anxiety and depression
-
Cognitive decline
-
Neurodevelopmental disruptions
-
-
Indian studies (NIMHANS, AIIMS) are exploring gut dysbiosis as a factor in psychiatric illnesses.
3. India’s Antibiotic Culture
-
Overuse & misuse: OTC sales, patient demand, fee-for-service prescription incentives.
-
Statistics:
-
AMR caused 2.67 lakh deaths in 2021 in India; projected to rise to 1.2 million by 2030. (IHME)
-
Nearly 50% of antibiotics consumed are unapproved formulations (Lancet, 2022).
-
-
Socio-cultural factors: Quick-fix mindset, low awareness, reliance on pharmacies in rural/semi-urban areas.
4. Mental Health Implications
-
Biological pathway: Dysbiosis → Inflammation (↑ cytokines IL-6, TNF-α) → altered neurotransmission.
-
Psychosocial dimension: Stress, anxiety, depression worsened by poor gut health.
-
Emerging therapy: Psychobiotics (probiotics & prebiotics) show promise in reducing depressive symptoms (Frontiers in Psychiatry, 2020).
5. Policy and Public Health Interventions
a) Education & Awareness
-
Embed gut-brain literacy in school curricula, NHM, and Ayushman Bharat programmes.
-
Campaigns on dangers of self-medication and importance of balanced diet (fermented foods, probiotics).
b) Regulatory Reform
-
Central Drugs Standard Control Organization (CDSCO): Strict prescription-only antibiotic policy.
-
Penalise pharmacies and practitioners violating norms.
c) Surveillance & Research
-
Strengthen INSAR (Indian Network for Surveillance of AMR) with integration of mental health metrics.
-
Invest in India-specific microbiome research to develop psychobiotic interventions.
d) Clinical Practice
-
Integrate antibiotic stewardship into medical education.
-
Encourage psychiatrists to include GI health assessments in evaluations.
-
Nutrition counselling as part of mental health care.
e) Leveraging Traditional Knowledge
-
Promote fermented foods (curd, idli, dosa, pickles) as natural probiotics.
-
Combine Ayush & modern psychiatry approaches for holistic care.
6. Challenges
-
Weak enforcement of drug regulations.
-
Low doctor-patient ratios, esp. in rural India.
-
Pharma–market linkages incentivising over-prescription.
-
Limited mental health infrastructure (India spends ~1.3% of GDP on health, <0.1% on mental health).
7. Conclusion
-
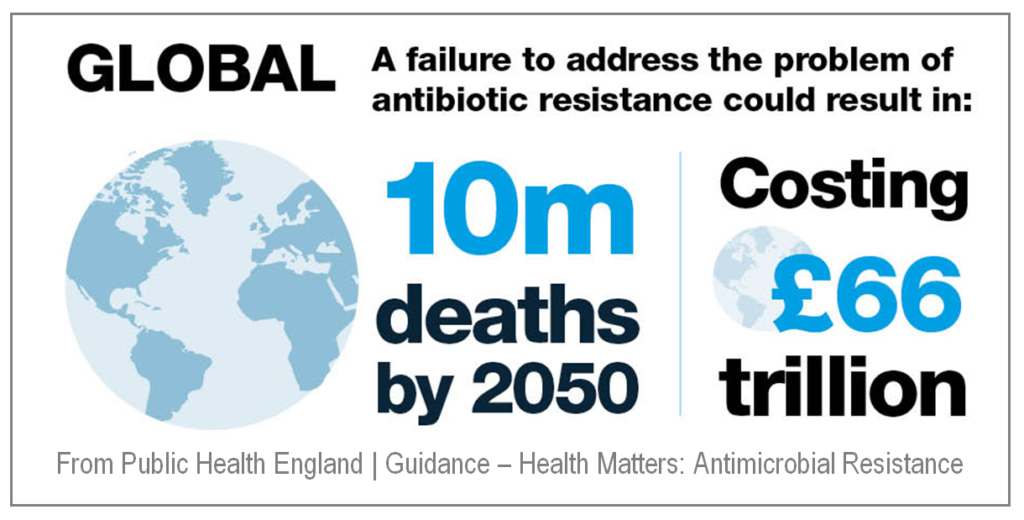
AMR is not just a physical health crisis but also a mental health crisis in the making.
-
India must adopt a One Health + Gut-Brain Axis perspective, integrating microbiology, psychiatry, nutrition, and public health.
-
With rising mental health burden and AMR fatalities, responsible antibiotic use + gut-friendly interventions are indispensable for sustainable health security.
